
Placental Cell Platform
Allogeneic placental cell-based platform to address unmet medical needs
PLACENTAL-BASED CELL PLATFORM
The placenta is a highly specialized organ that develops during pregnancy and is vital in supporting fetal growth and development. In addition, it acts as a barrier between the mother and fetus, allowing the exchange of nutrients, oxygen, and waste products.
It has been discovered that the placenta contains a variety of cells, tissues, and molecules that have great potential for use in regenerative medicine.
Placenta contains mesenchymal stromal cells, which can potentially regenerate damaged tissues. Among the molecules in the placenta are growth factors that promote cell growth and division and stimulate the regeneration of damaged tissues. Additionally, cytokines, small proteins that regulate immune responses, can modulate the immune system and promote tissue regeneration.

Solid immunomodulatory potential in peripheral blood mononuclear cell co-culture, indicating that it can regulate and modulate immune responses
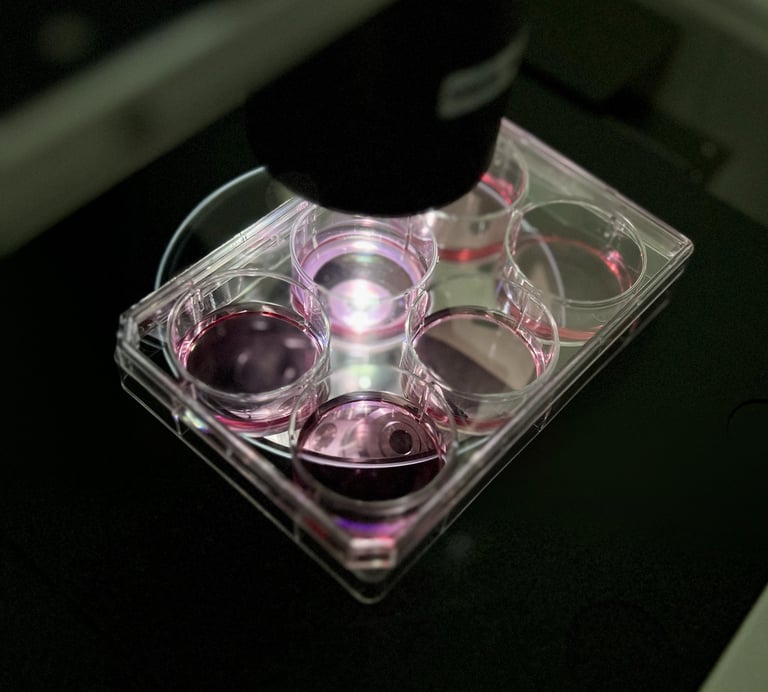
Platform Extensive in vitro characterization
High yields and viability indicate it is a robust and reliable cell source
Mesenchymal stromal cell markers, and lack of HLA, suggest they are immunocompatible
The lack of senescence indicates a young cell population with good proliferative capacity
Karyotype is stable, indicating that the product does not exhibit chromosomal abnormalities
Through years of placenta-based research and development, we have created an advanced cell platform exhibiting a potent mode of action. Together with partners, Keli Therapeutics has utilized the knowledge and leveraged the experience in:
stromal cell physiology and biology
upstream and downstream bioprocess development
quality controlled manufacturing
GMP / GLP regulatory affairs
KELI Therapeutics has led a series of non-clinical studies showing the cell platform's safety and efficacy in vitro and in vivo. We are investigating KELI-100 as a treatment for multiple indications: Acute Kidney Injury, Acute Respiratory Distress Syndrome, Skin Neutrophilic Dermatosis and Osteoarthritis.
WE LEVERAGE THE KNOW-HOW TO DEVELOP NEXT-GENERATION CELL THERAPIES


ACUTE KIDNEY INJURY
Acute Kidney Injury (AKI) is the most common post-cardiac surgery complication. AKI is a condition in which the cells in the kidney tubes are injured (due to multiplex pathophysiology, primarily inflammation, cell death, and oxidative stress).
Our KELI-101 program has shown positive effects in managing AKI by improving survival rate, serum and urine biochemistry, and preventing structural chronic kidney injury.
KELI-101 is currently being investigated in a clinical Phase 1b/2 clinical trial.
Improved the survival rate of animals
Promoted and sustained normal diuresis, indicating that the kidneys can produce and excrete urine at a regular rate
Improved biochemistry and electrolyte balance in urine and serum, indicating a preserved kidney function
Reduced inflammation and oxidative stress in the kidney, indicating prevention of AKI
Reduced structural damage preventing tubular dilatation, acute tubular necrosis, cast formation, loss of brush border, interstitial fibrosis, and tubular atrophy indicates a long-term protective effect on the kidney structure.
OSTEOARTHRITIS AND SYNOVITIS
Osteoarthritis (OA) and synovitis involve complex pathophysiological processes, including inflammation, cell damage, and oxidative stress, affecting the overall health and function of the affected joints.
KELI-102 program has shown promising results in managing OA and synovitis by promoting tissue repair, reducing inflammation, and improving joint function.
Displayed marked improvement in gross changes of OA, such as cartilage osteophytes and subchondral bone exposure
Reduced the formation of fissures on the surface of the femoral condyle, indicating better preservation of articular cartilage
Decreased the expression of inflammatory markers in the treated group synovium, indicating suppressed inflammation
ACUTE RESPIRATORY DISTRESS SYNDROME
Acute Respiratory Distress Syndrome (ARDS), marked by lung inflammation and impaired gas exchange, results from a dysregulated pulmonary inflammatory response triggered by various factors. The initial insult releases pro-inflammatory cytokines, activating lung endothelial cells and increasing alveolar permeability. Circulating leukocytes, such as neutrophils, macrophages, and lymphocytes, contribute to tissue injury by releasing additional pro-inflammatory mediators.
KELI-103 program seeks to manage ARDS by reducing inflammation, promoting lung repair, and preventing fibrosis by suppressing the activation of pro-inflammatory cytokines.
Reduced inflammatory cytokines and chemokines in bronchoalveolar lavage (BAL) fluid, indicating suppressed lung inflammation
Reduced protein concentration in lavage fluid, suggesting a decrease in lung edema and permeability
A reduced number of neutrophils, macrophages, eosinophils, and basophils in BAL fluid, indicating reduced inflammation, prevention of lung tissue damage, and improved oxygenation
Reduced structural alveolar damage, consolidation, and inflammation, indicating a more favorable environment for repair and regeneration
Downregulated inflammatory gene expression of lung tissue, indicating a reduction in lung damage and promotion of repair
NEUTROPHILIC DERMATOSIS
Neutrophilic dermatoses are a group of disorders characterized by skin lesions in which neutrophils, a type of white blood cell, are the primary component. Hidradenitis suppurativa (HS) is one of the representatives of neutrophilic dermatoses. HS, or acne inversa, is a chronic inflammatory skin condition causing significant socio-economic impact. HS is characterized by painful, pus-filled lumps in areas such as the armpits and groins. These lumps lead to scarring, severe pain, and movement restriction, profoundly affecting quality of life.
Current treatment options are limited and rarely curative.
KELI-104 program seeks to manage and modulate the aberrant immune response and alleviate skin inflammation.
Suppressed stimulated HS patient lymphocyte proliferation
Reduced the relative number of HS patient cytotoxic lymphocytes
Increased secretion and gene expression of IL-10 in HS patient lymphocytes and skin explants, which shows a shift towards an anti-inflammatory response
Reduced secretion and gene expression of various pro-inflammatory cytokines in HS patient lymphocytes and skin explants
